 Regeneration of Beta Cells by Natural Remedies – Cresvin Beta
Regeneration of Beta Cells by Natural Remedies – Cresvin BetaReversing Diabetes Waking Beta Cells— Almost there. The potential for remission in newly diagnosed diabetes seems feasible because changes in the beta cell function can lead to disease remission for type 1 diabetes and type 2 diabetes inverse. With Roy Taylor, MD, Michael Haller, MD, Domenico Accili, MD and J. Michael Gonzalez-Campoy, MD, PhDWith 1.5 million Americans who learn that they have diabetes annually, the push to reverse diabetes has taken a promising turn given results from several recent studies. 1-3Roy Taylor, MD, medical professor at Newcastle University, UK, continues to investigate type 2 diabetes (T2D), further demonstrating that newly diagnosed patients can reverse the disease with substantial weight loss1,2 In the last study published in Cell Metabolism2, Dr. Taylor and his team presented new clues about how weight loss can be responsible for improving the beta cell function in some individuals, and why others who lost substantial amounts of weight could not shed their diabetes. In a trial focused on type 1 diabetes (T1D),3 Michael Haller, MD, medical professor and head of pediatric endocrinology at the University of Florida Institute of Diabetes in Gainesville, reported that low-dose anti-timocyte blood (ATG) blood cell function preserved and improved hemoglobin A1c (HbA1c) in patients with new T1 cells. Indeed, Dr. Taylor told EndocrineWeb, his weight loss program is ready for the first time, so it is very important that doctors be prepared to be more aggressive about weight loss stress in patients than recently diagnosed with type 2 diabetes, while Dr. Haller said his approach still requires more research with longer follow-up before any celebration can begin. Results of the Primary Care Weight Loss Program In an essay published in Lancet,4 Dr. Taylor et al reported that almost half of the patients who were followed with early T2D were able to return to non-diabetic state after substantial weight loss. Since this data was presented, researchers have been going to test the hypothesis that weight loss of more than 10 kg (22 pounds) would normalize liver fat and reduce pancreatic fats, so that an investment in the state of diabetes seemed to depend entirely on the ability of each patient's beta cells to recover after dramatic changes in body weight. 1 Researchers are closing in agents that appear to increase the function of beta cells in people with type 1 diabetes. Our work,1.2.4 Dr. Taylor said, "retouch the long-standing belief that beta cell function is lost irreversibly in patients with type 2 diabetes. In fact, beta cell activity can be rescued, he said, based on his research by examining potentially relevant metabolic factors, such as liver fat content, pancreatic fat levels, triglycerides and beta cell function in a subset of 64 patients from the previous study. In the intervention group,1 liver fat content decreased from 16% to 3.1% (P = 0.0001).2 Among patients with a very low dietary plan in calories, plasma triglycerides and pancreas fat decreased regardless of their glucose activity. In addition, both in those who responded and in those who did not, the reduction of metabolic factors was similar, but only the response teams showed early and sustained improvements in the beta cell function. 1.2The most striking difference was the first-phase insulin response2, according to Dr. Taylor, as it increased in response teams but not in which they are not responsible.1 The recovery of the first phase insulin response (0.04 to 0.11 nmol.min/m2, P = 0.0001) defined those who returned to the non-diabetic state and was durable at 12 months. It is also important: good response teams generally had a shorter duration of diabetes (2.7 years vs. 3.8 years, P = 0.02). "As you would expect, people had a different length of the window as to when they remained reversible [with respect to their diabetes]," said Dr. Taylor endocrineWeb. For example, a patient had been diagnosed with diabetes for 24 years, he said, and returned to the normal insulin function. 'It seems that this person had beta cells susceptible to being quenched by the accumulation of fat that was not quite kaput by fat.' While this patient may be a chess, "for others, even three years [after diagnosis] was too late," he said. These study results advance our understanding of the start of type 2 diabetes by moving the clinical field closer to the possibility of a cure, at least in some people1, said Dr. Taylor. "T2D is simply the result of too much fat overloading the liver and pancreas in people who turn out to be susceptible to fat-induced damage," he said. A limitation of the study, however, is that the population sample was 98% of the Caucasus, so similar research is essential in other populations, as is more follow-up, and this is underway. Plan of Action in Clinical Practice Although there are many questions left, Dr. Taylor expressed the certainty that time is suitable for endocrinologists and primary care doctors to take a more aggressive approach to the weight of their patients — more urgently in those who are recently diagnosed with type 2 — to emphasize the urgency of losing excess weight immediately. While about half of their patients were happy to take antidiabetes medications to manage their blood sugar despite known complications of diabetes, Dr. Taylor said, many others were "horrified" by receiving a diagnosis of diabetes, and they seemed highly motivated to address the condition. Clinicians should find relief security that patients expressed by learning that a lifestyle change could be sufficient to reverse the course of their disease. "Health care providers can learn this [weight loss] protocol with just eight hours of training," Dr. Taylor said. However, he said it was prudent for doctors to select patients wisely, as his recommended approach to weight control is "not for the weak of the heart: The initial three-month weight loss stage is a liquid diet—four shakes a day, 200 calories each. "After the weight loss phase, patients are transferred back to regular meals, replacing a smoothie at a time to gradually restore solid foods, as the patient receives individualized instructions on how to eat to keep the weight lost.2 Participants were seen once a month to receive individualized weight maintenance guidance, including eating instructions about 30% less than their estimated consumption at the beginning of the study. 4Another key aspect of Dr. Taylor was working with patients who successfully achieved the desired weight loss to the exercise phase as an important element of the weight-maintenance phase. "A few people took a sport they used to play," he said. Or in many cases he just started walking daily. Even so, "the average weight tended to rise" among many of the participants," he said, speculating that the difficulty of maintaining the lost weight can depend on the personal thresholds of 'grase'." Indeed, it may be that when the weight of fat starts to increase in patients who have successfully reversed their diabetes diagnosis, keeping an eye on liver fat levels can provide a key to future treatment strategies in these patients, Dr. Taylor. An explanation for the development of type 2 diabetes may be that people with a so-called healthy body mass index may be carrying more fat adipose that their body is able to cope to prevent diabetes, said Dr. Taylor. Reversing the natural history of type 1 diabetes, too much. In research focusing on T1D,3 Michael J. Haller, MD, professor and head of pediatric endocrinology at the University of Florida, Gainesville and colleagues, found that the treatment of newly diagnosed patients with type 1 diabetes with low-dose anti-timocyte globulin (ATG) slowed down the peptide C and reduced hemoglobin A1c (HbA1c). "We use FDA-approved drugs and repurpose them for use in T1D," Dr. Haller endocrineWeb, so far, ATG has been used primarily to treat kidney transplant patients. According to their findings published in Diabetes Care,3 researchers focused on understanding that type 1 diabetes is a mediated T-cell process marked by the autoimmune destruction of β cells, he said. While several agents targeting T and β lymphocytes have demonstrated their promise, no agent has demonstrated long-term or sustained success in preserving peptide C or reducing HbA1c, which are two critical indicators of disease reversal. His team randomly assigned 89 patients, with an average age of 17 years, who were diagnosed with type 1 diabetes for less than 100 days, to one of three groups:3 The average measurement of one year of peptides C (according to the assessment of the concentration of plasma drugs under the curve) was significantly higher in those of the first group: treated with ATG (0.646 nmol/L) versus placebo (0.406 nmol/L, P = 0.0003), but not in the treaties with the combination (0.528 nmol/L) versus placebo (P = 0.031).3 Both ATG alone, as well as the ATG and GCSF combination, achieved a reduction in A1C a year. "Of course, a longer follow-up is necessary to see if the findings hold," said Dr. Haller, "and it will be critical to evaluate the effectiveness of maintenance therapy." Although it still does not propose that doctors try treatment with patients at this time, he said that findings offer a reasonable promise that type 1 diabetes can be reversed or even prevented on a large scale. Closure in the biological mechanisms of beta cell action Patients in the diabetes community '' have been talking for some time about the understanding that in diabetes, mainly for type 2, insulin producing cells are not dead but simply inactive," said Domenico Accili, MD, head of the endocrinology division, and Diabetes professor of Russell Berrie Foundation in the New York University College of Physicians. Accili, so "if you put patients with diabetes in a diet [to promote weight loss], it will have a positive impact on their beta cells." To reiterate Dr's feeling. Taylor, "The message for patients is to change their lifestyle when you get a type 2 diabetes diagnosis. With this recent research, "what we are learning now is, perhaps there is more room for changing the lifestyle of what we think, and with a much more significant impact," said Dr. Accili in EndocrineWeb. He also said, "The Haller study goes in that direction, suggesting that intervention in the early stages of type 1 diabetes could also make a difference." Dr. Accili agreed that ''this is not yet in the clinical stage' for type 1 diabetes, but it's worth going on. Insights from Experts in Obesity Management "Both studies are of significant interest," promoting our understanding of the relationship between obesity and diabetes, said J. Michael González-Campoy, MD, PhD, FACE, medical director and CEO of the Minnesota Obesity Center, Metabolism. "First, we know that with the increase of fat mass can develop dysfunction of adipose tissue (i.e., adiposopathy). Changes in adipent hormones—specifically an increase in leptin and a drop in adiponectin, and the development of insulin resistance by which insulin cannot activate its receptor in target tissues—will have a negative impact on beta cells. In particular, as insulin resistance also develops the inability to move triglycerides in cells, which makes the body recurs free fatty acids, which directly harms beta cell function. This process establishes a vicious cycle, with the decrease in insulin release leading to a greater decrease in insulin activity that then leads to an additional increase in circulating triglycerides," said Dr. Gonzalez-Campoy. "In terms of weight loss, it is evident that some patients are more sensitive and able to restore their insulin production, while others cannot recover. It might be that the response teams could restore the first phase of insulin release to increase insulin production, but the action mechanism for this difference was not captured in this document. Although triglycerides fell into both groups, there were differences in VLDL-triglyceride levels, and this offer at least a partial explanation," he said. "However, the [Taylor] document on type 2 diabetes did not measure adipokines or levels of intestinal hormones," said Dr. González-Campoy in EndocrineWeb. As such, there are other mechanisms to be considered in managing diabetes. In adiposopathy, for example, the relationship of leptin to adiponectin increases (increasing leptin and decreases of adiponectorine); there are also elevations in markers of inflammation, since adiposopathy includes the infiltration of adiposo tissue by macrophages when adipose tissues exceed the vascular supply and ischemia is developed, Therefore, the need for additional studies to clarify the mechanisms of action to restore beta cell function," said Dr. Gonzalez-Campoy. "As for type 1,3 study, it is known that 'someone triggers an immune system response that leads to the development of antibodies against pancreatic beta cells. However, the trigger or triggers have not been identified, it seems clear that a population of lymphocytes capable of making antibodies against beta cells is involved," he said, adding, "The concept we can fight against this immune response is not new; now there are many monoclonal antibodies incorporated into the mainstream of medical practice." "The new thing is that those who were able to demonstrate that anti-timocitis globulin (ATG) decreased the beta cell loss rate in T1D patients while the addition of GCSF did not improve the protective effect of ATG," said Dr. Gonzalez-Campoy, "So, an immune attack that destroys the insulin-producing beta cells has proven to be a viable treatment. "Although we buy patients some time without the need for a complete insulin replacement, we are still not able to stop the destruction of beta cells," he said. "As the authors conclude, more studies will be needed to see if the therapy combined with ATG and other inmunitary modulators can stop the attack on beta cells." Lifestyle Strategies To Help Motivated Patients Nutrition experts have long claimed that a varied diet would be the route to improve health, but a more honest evaluation of the Western diet can put that axiom in your head. According to an American Heart Association scientific adviser published in Circulation, the clearest view of growing obesity and diabetes rates can be attributed to the wide variety of food products available to American consumers.5 According to Marcia C. Oliveira Otto, PhD, assistant professor at the University of Texas Health Science Center in Houston, for researchers who conducted a diet study analysis, "The long-standing recommendation of American public health to "eat a variety of foods" was introduced last century in response to widespread nutrient deficiencies, especially in low-income countries with limited access to nutritious food," Otto said. However, "the recent evidence suggests that this approach cannot help improve people's eating habits, or prevent obesity in places where processed and unhealthy food choices are very common, wide-ranging and relatively cheap." They concluded that on the present day, eating a wide range of foodstuffs has led to a scenario in which the American diet, composed of so many highly processed products and fast food, has led to an increase of 40% in over consumption and bad choices. 5 It is clear that the more choices there are, the more people eat. For example, it becomes a second nature for many to sit at a meal consisting of chips with ketchup and a smoothie or drink to go along with the cheeseburger in a white bread. In addition to the insult to the injury, when faced with a spread of cheap foods, the usual course is to finish each last part, so the concept of satiety has been lost. In fact, in front of the options corridors it has made it almost impossible for most Americans to make healthy food decisions. In another timely statement published by Houston Methodist Leading Medicine, Kristen Kizer, RD, a licensed clinical dietitian, said, "we live in a society that believes that lower calorie feeding means more weight loss and ultimately better health. While this is true in some respects, to succeed in both losing weight and keeping it out, it is [more] important to focus on the nutritional value, not only the caloric value, of its food." When faced with a newly diagnosed patient with diabetes, doctors can call these rational understandings to start a conversation about diet and weight management. To offer concrete strategies in response to "what I do now," here are some strategies to offer (with links to direct your patients for more reading): There is no relevant financial information for any of these professionals except. Dr. Accili, co-founder of a biotech company, Forkhead Bio Therapeutics, which is involved in developing diabetes treatments. Endocrine Research UpdatesProfessional resourcesPolitics and ContactSubscribe to "Endo Monitor", eNewsletter endocrineWeb for HCPs
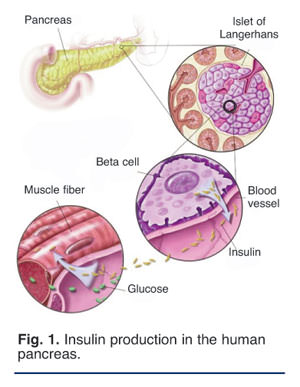
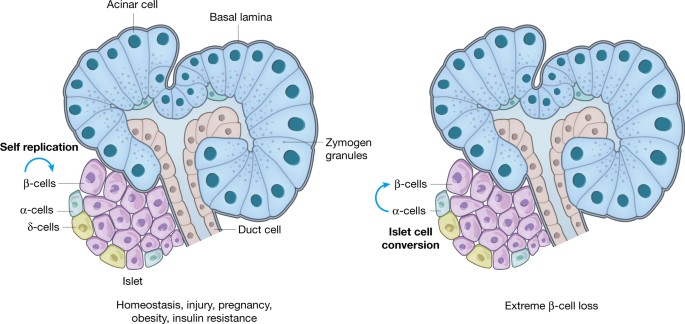
HemorrhoidsDiabetes (Type 1 and Type 2) Jock Itch Vyvanse vs. StratteraBenzodiazepinesZoloftLow Fiber DietAerobic ExerciseProbiotics Adults skin conditions Common eye problems and infections Sexually transmitted diseasesDiet and Nutrition QuizHeart QuizKidney Disease QuizKidney DiseaseCharacteristics of Alopecia Disease Areata©1996-2020 MedicineNet, Inc. All rights reserved. MedicineNet does not provide medical advice, diagnosis or treatment. . / / / / cells beta insulin producers can rebirth article Study discovers that beta cells that produce insulin can be rebornLatest Diabetes NewsBy Serena GordonSUNDAY, April 4 (HealthDay News) -- Certain pancreatic cells can be regenerated in insulin-producing cells after normal insulin-producing cells have been destroyed, as in type 1 , a new found study. Swiss researchers discovered that when they destroyed insulin-producing cells, known as beta cells, in mice to induce an artificial form of , other pancreas cells called alpha cells and then changed into insulin-producing beta cells. "The adult pancreas can regenerate new beta cells even if they are totally absent - as in," said the senior author of the study, Pedro Herrera, professor in the cell physiology department and metabolism at the Faculty of Medicine at the University of Geneva. Experts warned, however, that much more research is needed to see if the process could benefit people with, an autoimmune disease in which the immune system attacks beta cells in the pancreas it produces, the hormone that allows people to convert food into energy. People with type 1 should rely on insulin therapy for the rest of the lives. And if such a process occurs in humans, or could be induced to occur, there is a large road barrier. In type 1 , the immune system attack on beta cells seems to continue indefinitely, so people who have had insulin cell transplants should eventually return to insulin. The immune system destroys transplanted beta cells as well. "Every time you're thinking of any kind of healing or really good treatments for type 1 diabetes, you have to consider both beta cells and the immune side," said Andrew Rakeman, the manager of the scientific program in beta cell regeneration at the Youth Diabetes Research Foundation (JDRF). JDRF funded a part of the new investigation. "At this point, it is unknown if the reprogrammed alpha cells would be vulnerable. Alpha cells are usually not destroyed by the immune system, but in regeneration, they are losing features that make alpha cells become beta cells. So they are likely to appear in the immune system as beta cells," Rakeman said. To induce type 1 diabetes in mice, Swiss researchers exposed rodents to a toxin that destroyed only their beta cells. Alpha cells are usually found in the pancreas next to beta cells. Alpha cells secrete a hormone called that counteracts the effects of too much insulin and helps the body maintain normal blood levels. More than 99% of beta cells were destroyed in mice. Researchers labeled alpha cells with a fluorescent protein so they could trace those cells. They found that when almost all beta cells had been destroyed, if insulin therapy was given to mice to keep them alive, alpha cells spontaneously became functional beta cells. After converting enough alpha cells into beta cells, insulin therapy was no longer necessary. The new research, published on April 4 in the online edition of Nature magazine, is the first to show that this change can occur naturally and spontaneously, said the authors of the study. The previous research has been able to change adult cells in insulin-producing cells, but that change requires genetic manipulation, which could hinder the development of a type of drug to reproduce the effect. Rakeman said what is exciting in this new study is that "reprogramming is something that can happen naturally. If one can delineate what is causing it to happen in mice, it might be possible to find interventions to induce it to happen in humans." Herrera said researchers want to learn more about how alpha cells experience this change, and they also want to know if other cells can undergo this type of conversion. Dr. David Kendall, scientific director and doctor at the American Diabetes Association, said: "Everything that talks about a potential source of new insulin-producing cells is quite exciting. "However," he added, "I always have cautious enthusiasm for such findings. Early promise is not always a guarantee, and a series of mouse findings have not translated well into human research." Copyright © 2010 HealthDay. All rights reserved. SLIDESHOWHealth Solutions From Our SponsorsRelated ArticleSugar Box: Tips for managing diabetes " Glucose LevelsLearn to better control your glucose levels by avoiding blood sugar changes. Beware of caffeine, spices, exercise, sleep, alcohol and stress as they affect blood sugar levels and increase complications of diabetes. Read more: Blood sugar: tips for managing diabetes " glucose levels ©1996-2021 MedicineNet, Inc. All rights reserved. MedicineNet does not provide medical advice, diagnosis or treatment. . Categories of Health Popular Health CentersMedicineNet

Can You Regenerate Beta Cells Naturally? - Pancreas Beta Cells - Diabetes Self-Management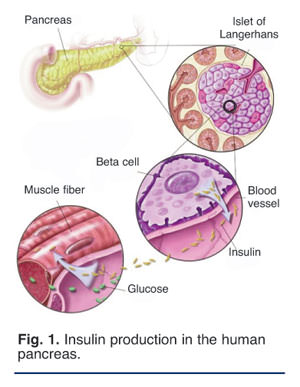
Cucurbita Pumpkin Rejuvenates ßeta Cells, Restores Insulin Production | Nutrition Review
Plant-Derived Compounds Targeting Pancreatic Beta Cells for the Treatment of Diabetes
Fasting-Mimicking Diet Promotes Ngn3-Driven β-Cell Regeneration to Reverse Diabetes: Cell
Plant-Derived Compounds Targeting Pancreatic Beta Cells for the Treatment of Diabetes
Can you grow new beta cells when your beta cells fail ? - BBC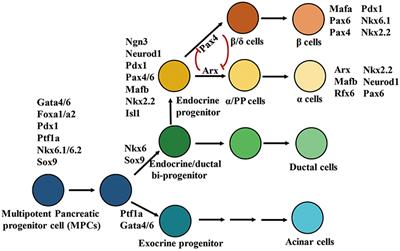
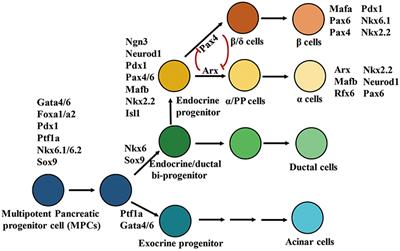
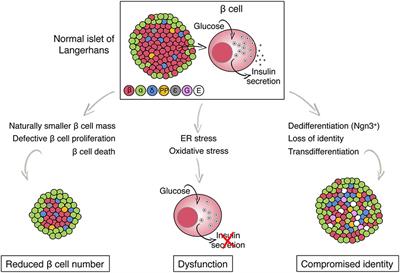
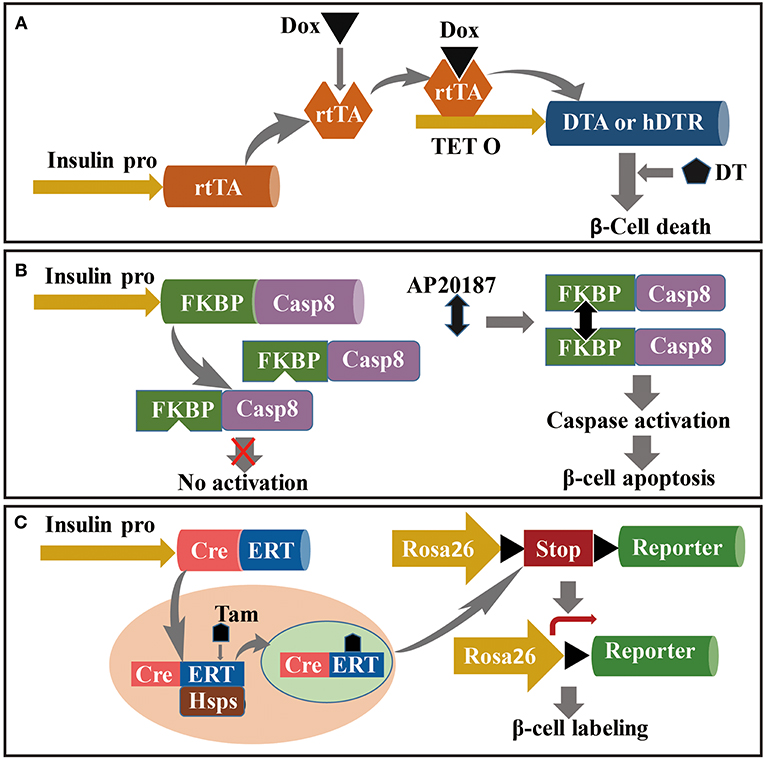
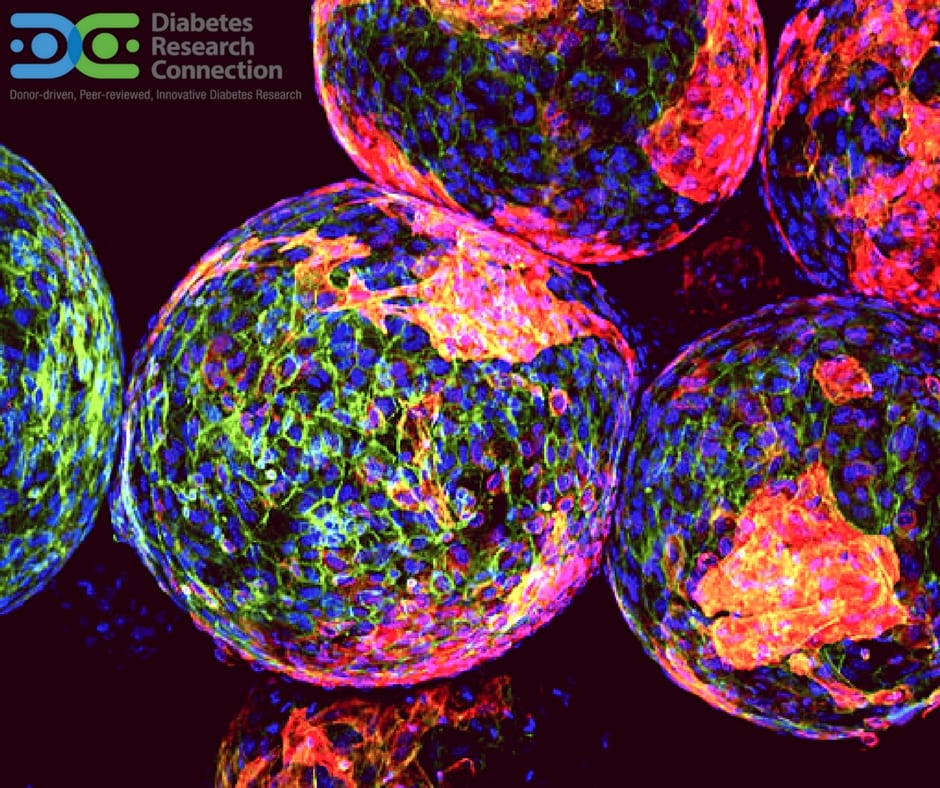
Frontiers | Endogenous Pancreatic β Cell Regeneration: A Potential Strategy for the Recovery of β Cell Deficiency in Diabetes | Endocrinology
GLP-1: Actions on Beta-cell Mass and Function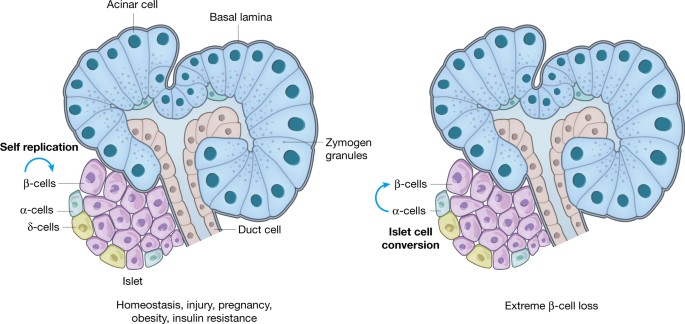
Pancreas regeneration | Nature
Cucurbita Pumpkin Rejuvenates ßeta Cells, Restores Insulin Production | Nutrition Review
Human Cell Regeneration, Brain Cell Regeneration, 6 Best Cell Regeneration Foods
Flavonoids for preserving pancreatic beta cell survival and function: A mechanistic review - ScienceDirect
An update on natural compounds in the remedy of diabetes mellitus: A systematic review - ScienceDirect
Can you grow new beta cells when your beta cells fail ? - BBC
Pancreatic stem cells have potential to regenerate beta cells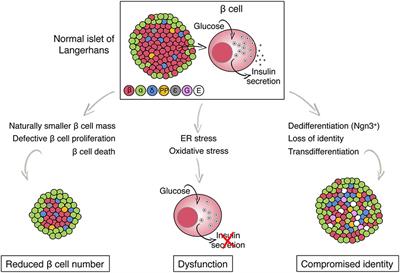
Frontiers | Metabolic Stress and Compromised Identity of Pancreatic Beta Cells | Genetics
Dapagliflozin promotes beta cell regeneration by inducing pancreatic endocrine cell phenotype conversion in type 2 diabetic mice - ScienceDirect
Bariatric surgery: beta cells in type 2 diabetes remission - Su - 2016 - Diabetes/Metabolism Research and Reviews - Wiley Online Library
Beta Cell Replacement Therapy | IntechOpen
Recent Insights Into Mechanisms of β-Cell Lipo- and Glucolipotoxicity in Type 2 Diabetes - ScienceDirect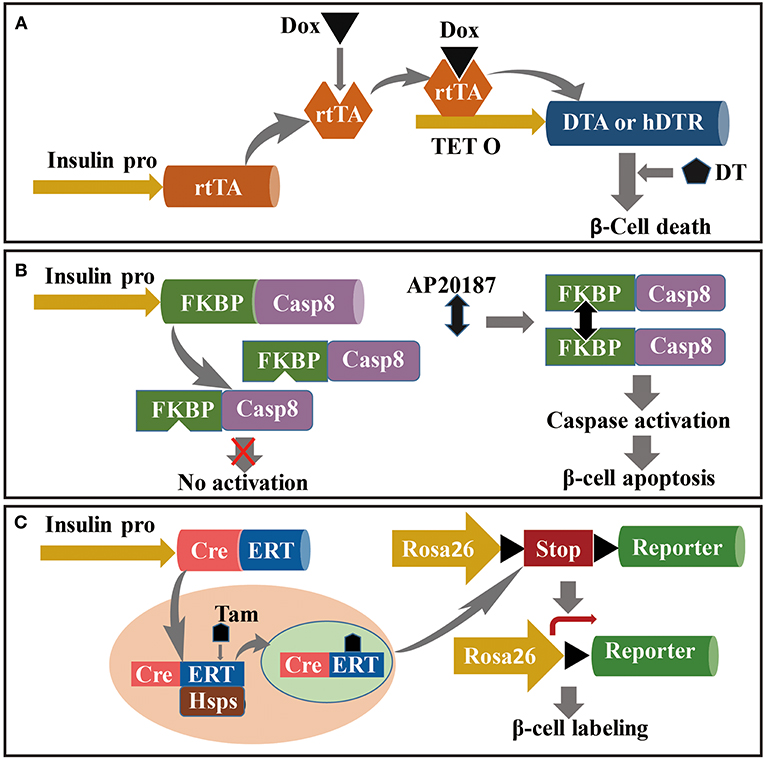
Frontiers | Endogenous Pancreatic β Cell Regeneration: A Potential Strategy for the Recovery of β Cell Deficiency in Diabetes | Endocrinology
Beta-Cell Regeneration: Definition and Overview - DSM
Antagonistic Glucagon Receptor Antibody Promotes α-Cell Proliferation and Increases β-Cell Mass in Diabetic Mice - ScienceDirect
Flavonoids for preserving pancreatic beta cell survival and function: A mechanistic review - ScienceDirect
Exploring Beta Cell Regeneration in Treating Type 1 Diabetes
Fasting-Mimicking Diet Promotes Ngn3-Driven β-Cell Regeneration to Reverse Diabetes: Cell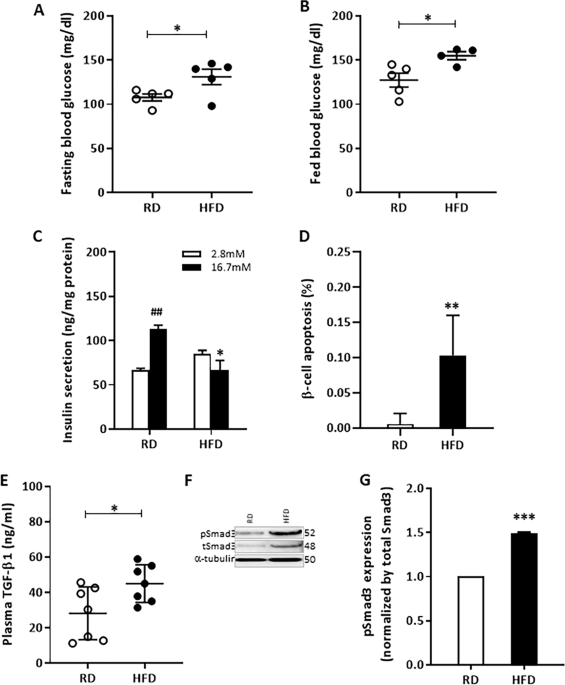
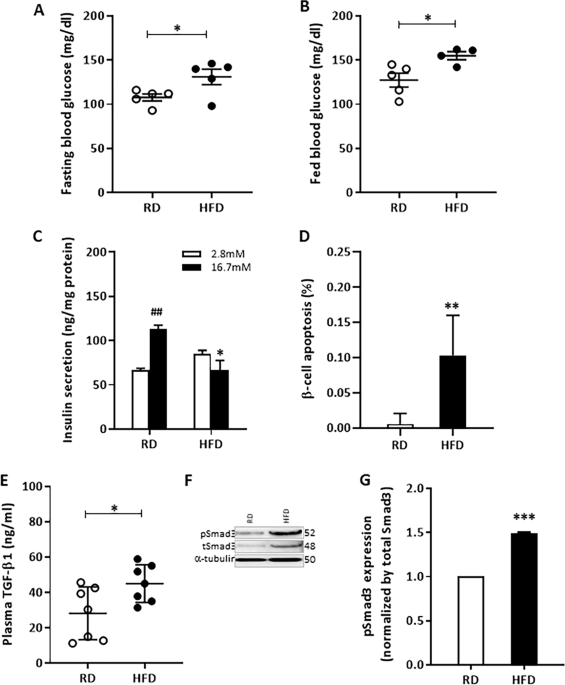
Protection from β-cell apoptosis by inhibition of TGF-β/Smad3 signaling | Cell Death & Disease
Mesenchymal stem cells ameliorate β cell dysfunction of human type 2 diabetic islets by reversing β cell dedifferentiation - EBioMedicine
Fasting-Mimicking Diet Promotes Ngn3-Driven β-Cell Regeneration to Reverse Diabetes: Cell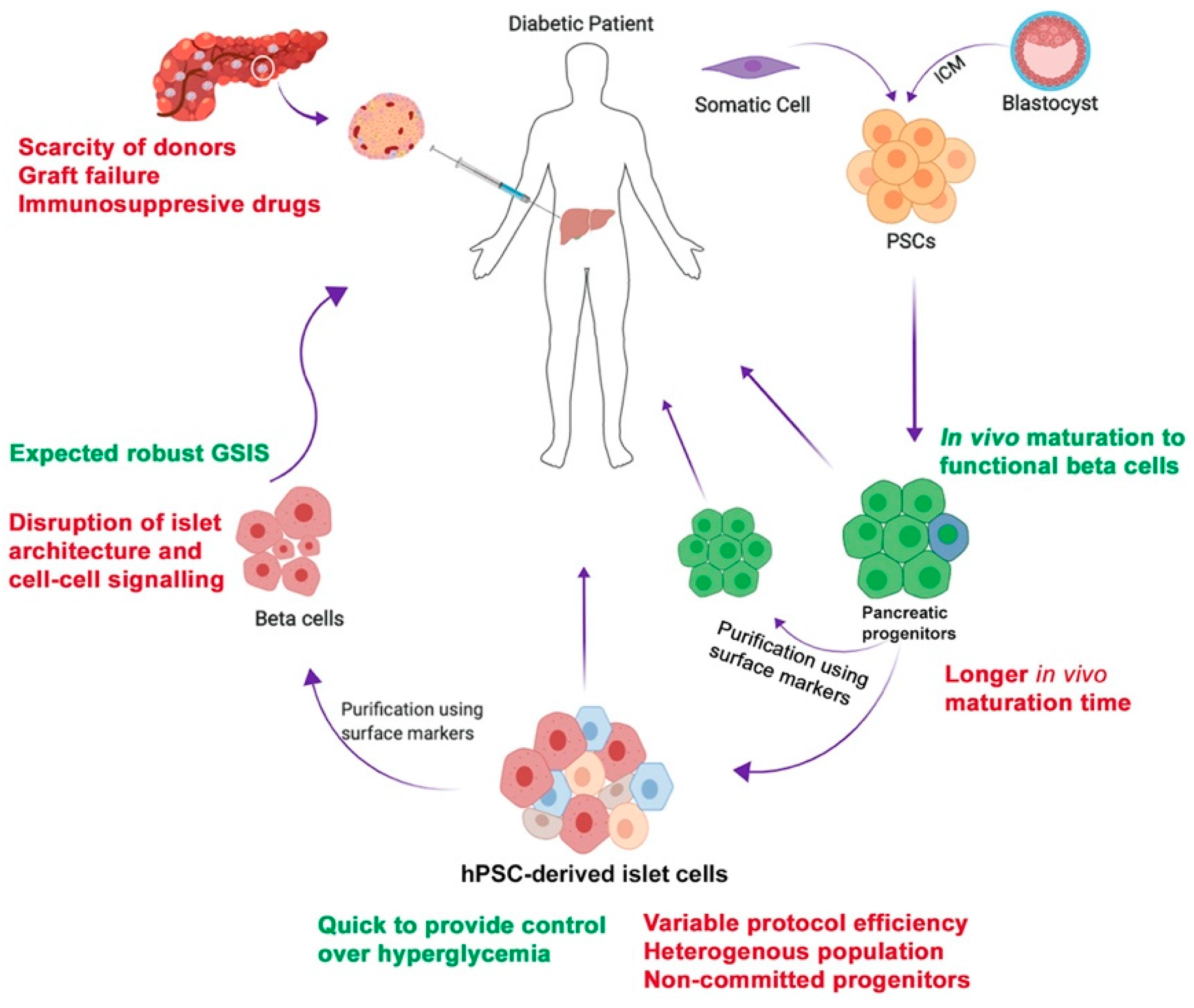
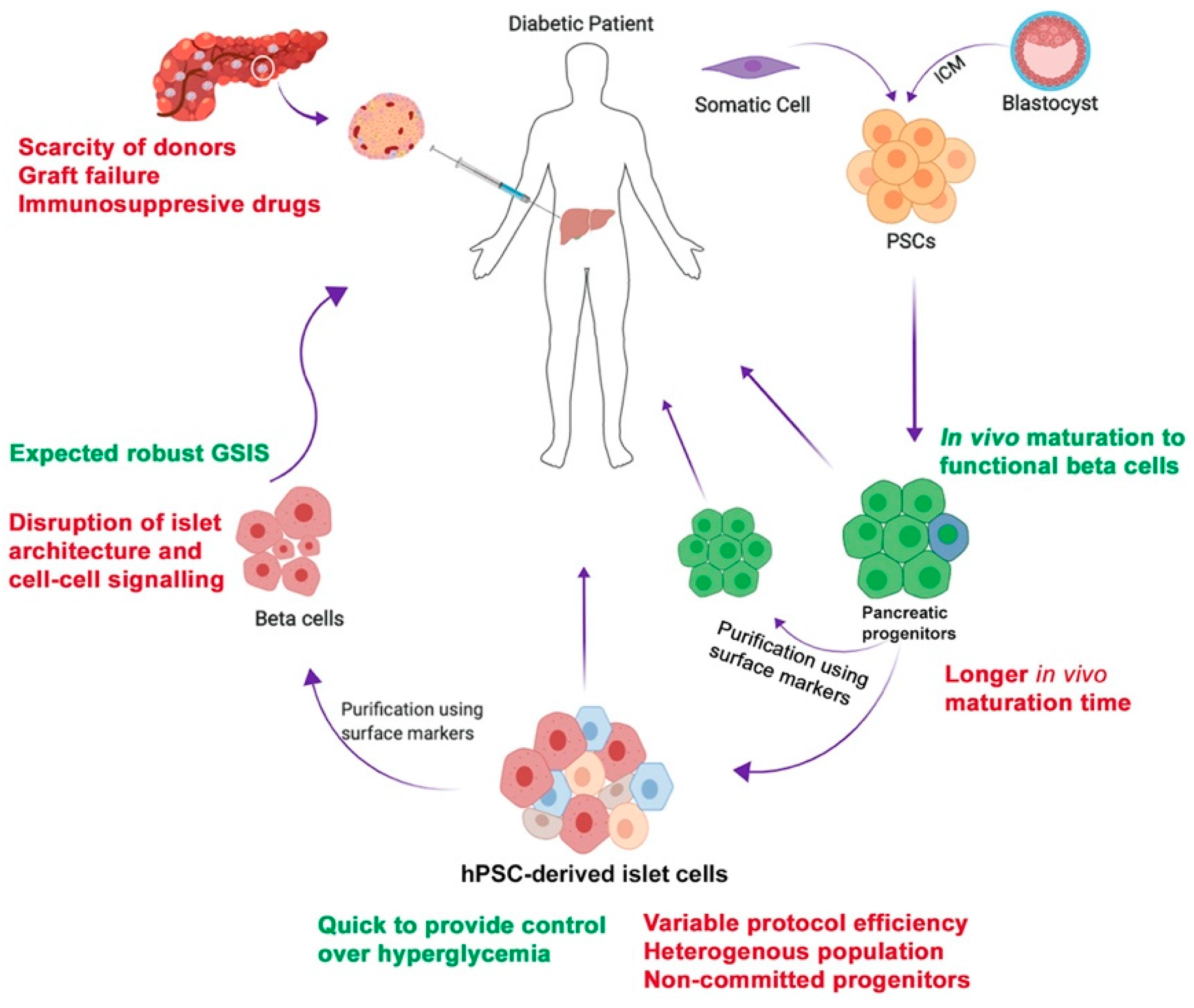
Cells | Free Full-Text | Stem Cell Therapy for Diabetes: Beta Cells versus Pancreatic Progenitors | HTML
Fasting-Mimicking Diet Promotes Ngn3-Driven β-Cell Regeneration to Reverse Diabetes | Reverse diabetes, Reverse diabetes diet, Reverse diabetes naturally
Beta cell - Wikipedia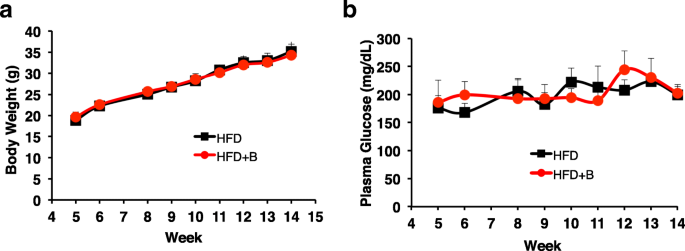
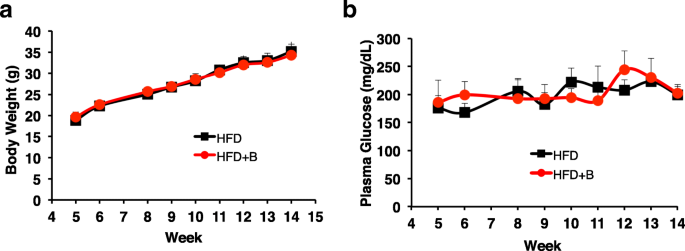
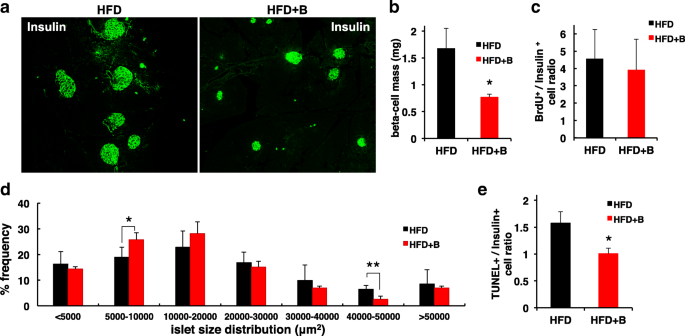
Whole blueberry protects pancreatic beta-cells in diet-induced obese mouse | Nutrition & Metabolism | Full Text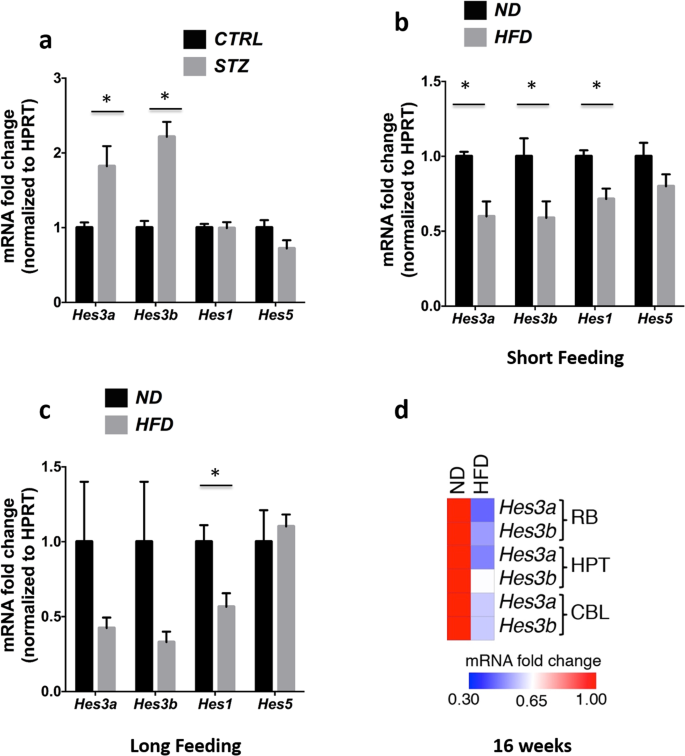
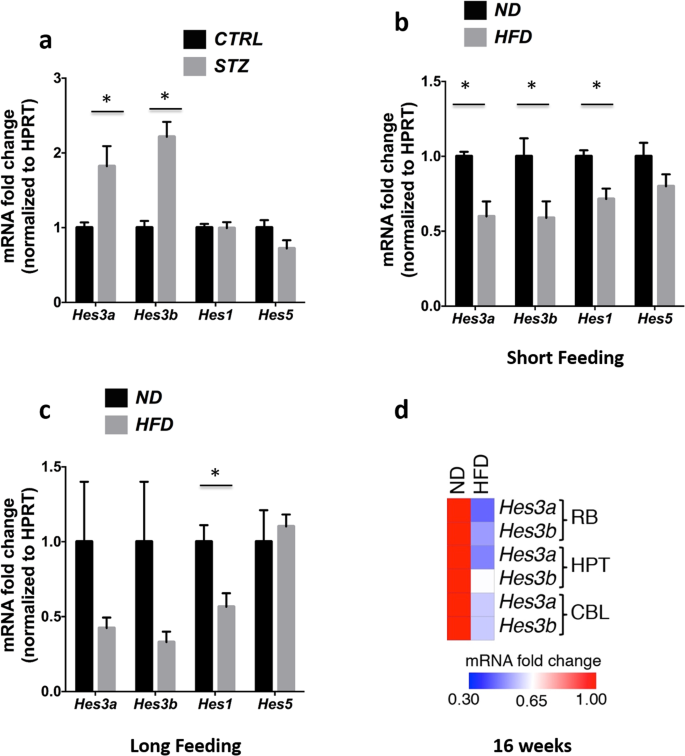
Streptozotocin-induced β-cell damage, high fat diet, and metformin administration regulate Hes3 expression in the adult mouse brain | Scientific Reports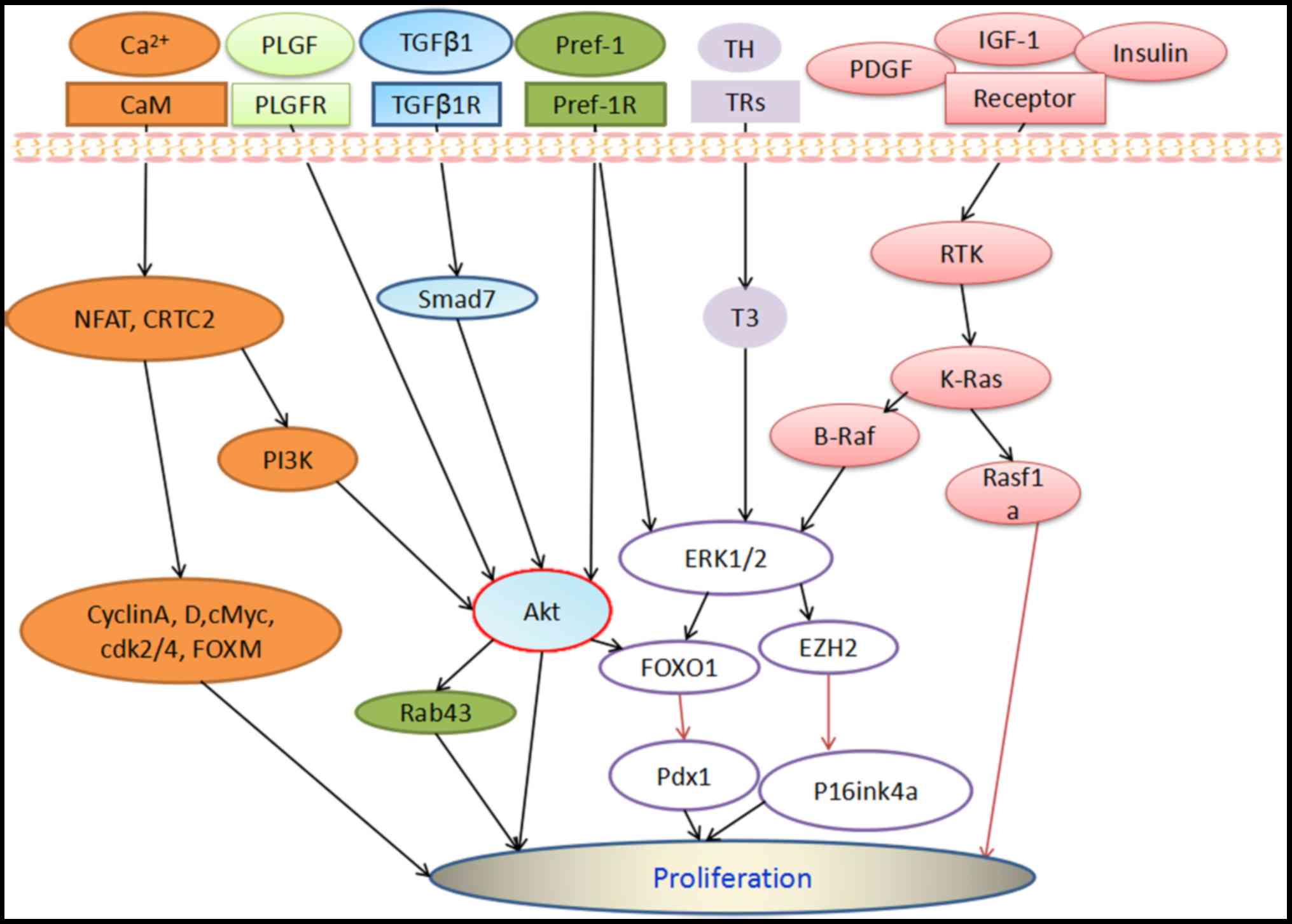
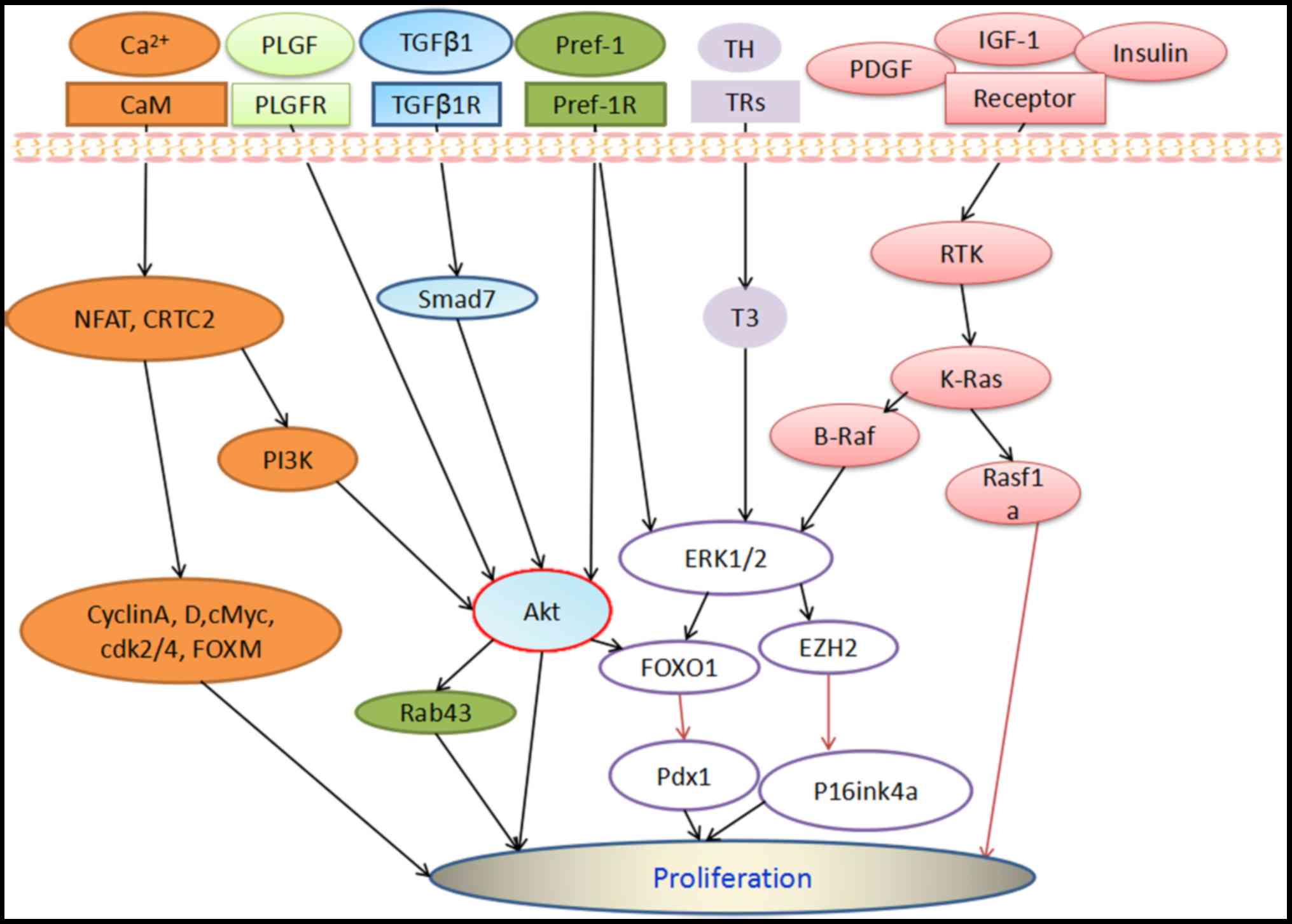
Cellular signaling pathways regulating β‑cell proliferation as a promising therapeutic target in the treatment of diabetes (Review)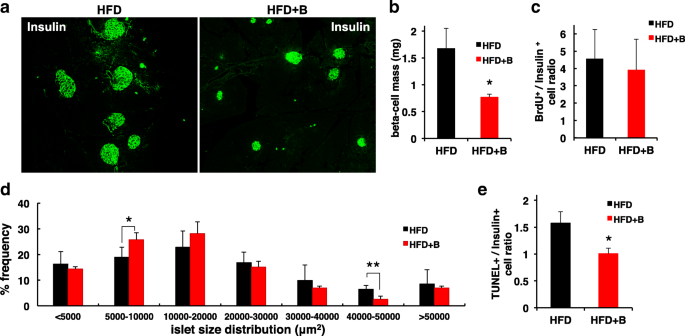
Whole blueberry protects pancreatic beta-cells in diet-induced obese mouse | Nutrition & Metabolism | Full Text
Can you grow new beta cells when your beta cells fail ? - BBC
Fasting-Mimicking Diet Promotes Ngn3-Driven β-Cell Regeneration to Reverse Diabetes: Cell
β-Cell Failure in Type 2 Diabetes: Postulated Mechanisms and Prospects for Prevention and Treatment | Diabetes Care
The Mastering Diabetes Blog – Learn the Science of Insulin Sensitivity


























Posting Komentar untuk "how to regenerate beta cells naturally"